Last Updated on 21 November, 2023
In recent years we have seen some of the prettiest and most beautiful cafes in London open up. Not only perfect for the Instagram shop but also serves up some amazing and delicious treats.
Among the many cool things to do in London is a trip to the lovely Instagrammable cafes in London you need to check out. So, if you’re looking for a gorgeous place to relish a cup of coffee or tea in London, here are some wonderful cafes that come highly recommended!


23 Instagrammable And Prettiest Cafes In London


Peggy Porschen Cakes
Peggy Porschen Cakes is located on Elizabeth Street in Belgravia, which is an upscale neighbourhood in central London.
The closest tube station is Sloane Square, but it’s also within walking distance of Victoria Station if you’re coming from elsewhere in the city.
In addition to being Insta-worthy on the inside and out, Peggy Porschen Cakes also offers delicious food and drink.
The menu features everything from chocolate cake and cookies to savoury quiche and sandwiches. And, of course, there’s a selection of teas and coffees to accompany your meal.
View this post on Instagram
Aubaine Selfridges
Tucked away in the corner of Selfridges on Oxford Street, Aubaine Selfridges is a little piece of France hidden in the heart of London. This beautiful cafe is the perfect place to exit the hustle and bustle of the city and enjoy a leisurely meal with friends.
Aubaine Selfridges is located on the ground floor of the iconic Selfridges department store on Oxford Street. If you’re not familiar with the area, Oxford Street is one of the most active shopping streets in London, so it can be a bit hectic.
However, once you step inside Aubaine Selfridges, you’ll feel like you’ve been carted to another world. The cafe is located towards the back of the store, so it’s relatively quiet and peaceful.

The best way to reach Aubaine Selfridges is by public transport. The cafe is situated right next to Bond Street tube station, so it’s very easy to get to.
If you’re coming from outside London, you can also take the train to Marylebone station and then walk to Selfridges (it’s about a 10-minute walk).
There are several things that make Aubaine Selfridges so beautiful. Firstly, it’s decorated in classic French style with chandeliers, mirrors, and velvet chairs.
Secondly, there’s an abundance of natural light thanks to the huge windows. And last but not least, there’s a gorgeous terrace where you can enjoy your meal al fresco ( weather permitting).
If you’re looking for a calm oasis in the heart of London, look no further than Aubaine Selfridges. This beautiful cafe is decorated in classic French style and has a stunning terrace where you can enjoy your meal al fresco.
With its convenient location and peaceful atmosphere, Aubaine Selfridges is the ideal place to exit the hustle and bustle of metropolis life and enjoy a leisurely meal with friends.
View this post on Instagram
Feya Cafe
Feya is a cafe located in three different areas of London – Bond Street, Knightsbridge, and Marble Arch.
Each location offers a unique atmosphere, but all three are united by their beauty and delicious food. Here’s a closer look at each Feya cafe.
View this post on Instagram
Feya on Bond Street
Feya on Bond Street is located in the heart of London’s shopping district. If you’re looking for a break from all the shopping, this is the ideal place to stop for a coffee and a bite to eat.
The cafe has a light and airy feel, with plenty of seating both inside and out. And of course, the food is delicious!

Feya in Knightsbridge
Feya in Knightsbridge is located just a short walk from Hyde Park. This location is perfect for people-watching – you can sit outside and enjoy the sunny days or cosy up inside by the fire on cooler days.
The menu features both sweet and savoury options, so there’s something that everyone can enjoy. And don’t forget to try one of their famous hot chocolates!

Feya at Marble Arch
Feya at Marble Arch is located near some of London’s most famous landmarks, including Buckingham Palace and Oxford Street. This cafe is perfect for people who want to investigate all that London has to offer.
The menu features both classic and contemporary dishes, so you’re sure to find something you’ll love. And if you’re looking for an afternoon pick-me-up, they have a great selection of teas as well.
No matter where you are in London, there’s a Feya cafe nearby that will suit your needs. Whether you’re looking for a brief bite before exploring the city or want to relax with a cup of coffee after a stressful long day of shopping, Feya has something for everyone. So next time you’re in London, be sure to stop by one of their three locations!
Jimmy Choo Cafe – Harrods
If you are looking for a luxury cafe in London then this is one not to miss. Located in the heart of London, the Jimmy Choo Cafe – Harrods is one of the most attractive and luxurious cafes in the city.
The Jimmy Choo Cafe – Harrods is located in the Harrods department store on Brompton Road in Knightsbridge.
If you’re coming from outside of London, the nearest train station is Knightsbridge, which is served by the Piccadilly line.

Whether you’re looking for a really quick bite or a leisurely meal, the Jimmy Choo Cafe is the perfect spot to indulge in a little luxury. As soon as you step into the cafe, you’ll be enveloped in a luxurious and chic atmosphere.
The decor is modern and sleek, with marble countertops, plush velvet chairs, and sparkling chandeliers. And, of course, there’s an impressive selection of Jimmy Choo shoes and accessories on display.
If you’re looking for a really unique dining experience, look no further than the Jimmy Choo Cafe – Harrods in London.
From its prime location to its luxurious atmosphere, this cafe is sure to please even the most discerning traveller. So what are you waiting for? Make your reservation today!
View this post on Instagram

Farm Girl
Nestled away in the bustling city of London is a cafe that’s worth seeking out: Farm Girl. With locations in Belgravia, Notting Hill, Fitzrovia, Soho and South Kensington, there’s bound to be a Farm Girl cafe close to you.
The first thing you’ll notice when you step into a Farm Girl cafe is the decor. With its rustic chic style, the cafes are filled with beautiful plants, vintage furniture and an overall cosy atmosphere.


The menu features healthy and delicious options such as avocado on toast, chia pudding and a selection of salads and sandwiches. There’s also a great selection of coffees, teas and juices to choose from.
In addition to being a fabulous place to enjoy a meal or snack, the Farm Girl cafes are also perfect for people-watching. Situated in some of London’s most popular neighbourhoods, the cafes offer a front-row seat to people-watching at its finest.
So whether you’re looking for a spot to enjoy a healthy meal or just want to people-watch in one of London’s most beautiful cafes, be sure to check out Farm Girl the next time you’re in the city.
View this post on Instagram
Sketch
If you’re looking for a truly unique experience during your stay in London, look no further than Sketch. This world-renowned café, located in the heart of the city, is like nothing you’ve ever seen before.
From its stunning interiors to its delicious menu, Sketch is sure to leave a lasting impression.
Sketch is centrally located in London’s Mayfair district, just a short walk from Piccadilly Circus and Oxford Street. If you’re taking public transportation, the nearest tube station is Green Park.


Upon arrival at Sketch, you’ll be immediately struck by the venue’s beauty. The café is spread out over several floors, each more gorgeous than the last.
Be sure to explore all of the different rooms, including the stunning Gallery where afternoon tea is served. And don’t forget to take plenty of pictures—Sketch makes for the perfect Instagrammable backdrop!
In addition to being visually stunning, Sketch also offers a delicious selection of food and drink. The menu changes frequently, but you can always expect seasonal British fare with a modern twist. There’s also an extensive wine list if you’re looking to pair your meal with a glass of vino. Trust us, you won’t be disappointed!


Whether you’re looking for an Insta-worthy location or simply wanting to enjoy a good meal, Sketch ought to be right there at the top of your list while visiting London.
With its convenient location and breathtaking interiors, it’s easy to see why this café has become such a popular spot among locals and tourists alike. Bon appetit!
View this post on Instagram
EL&N Cafe
EL&N Cafe in London is a beautiful cafe located in the heart of the city. The cafe is situated on Wardour Street, close to Oxford Street and Tottenham Court Road. It is easily accessible by public transport and is also within walking distance of many of the city’s attractions.


The cafe is decorated with leather sofas and armchairs and large windows which allow natural light to flood in. The menu offers a broad variety of food and drink options, including breakfast, lunch, and dinner. There is also an amazing selection of cakes and pastries on offer.
The beauty of EL&N Cafe lies in its simplicity. It is a spot where people can come in to relax and escape the busyness of the city. The furnishings and leather sofas support in trying to create a feeling of luxury, while the large windows allow customers to take in the natural light.
View this post on Instagram
Minnow
If you’re ever in London and looking for a beautiful and hidden cafe to spend an afternoon, look no further than Minnow Cafe in Clapham. This charming cafe is the perfect spot to relax with a cup of coffee and a good book or to catch up with friends over brunch. Here’s everything you need to know about Minnow Cafe.
Minnow Cafe is located in Clapham, which is in south London. To get there, you can take the Northern line on the London Underground to Clapham North station, or you can take a bus from Brixton station. Once you’re in Clapham, Minnow Cafe is just a short walk away.
There are plenty of reasons to love Minnow Cafe. First of all, the food is absolutely delicious. The menu features classic British dishes with a twist, like avocado toast with poached eggs and smoked salmon, and there are plenty of vegan and vegetarian options available as well.
Secondly, the cafe has a gorgeous garden that’s perfect for enjoying a sunny day. And last but not least, the staff are always friendly and welcoming, making sure that every customer has the same great experience.
View this post on Instagram
The Knot Churros
Are you in the mood for something a bit sweeter? Something savoury? How about both? The Knot Churros Cafe in Kensington, London, has got you covered. This cafe is known for its churros – fried dough pastries that can be dipped in melted chocolate or savoury sauces. Yum! But The Knot Churros Cafe is much more than your sugar fix. It’s also a beautifully designed space that’s perfect for enjoying a cup of coffee or tea with friends.
The Knot Churros Cafe is located in the heart of Kensington, London. If you’re not familiar with the area, Kensington is a district in West London that’s known for its high-end shops and restaurants. The cafe itself is situated on High Street Kensington, which is one of the main shopping streets in the area.
The best way to get to The Knot Churros Cafe is by public transport. If you’re coming from Central London, you can take the tube (subway) to High Street Kensington station. The cafe is just a short walk from there. If you’re coming from elsewhere in London, you can use the TfL Journey Planner tool to find the best route by public transport.
On the inside, you’ll find an abundance of natural light and stylish furnishings. Whether you’re enjoying a cup of your favourite coffee at one of the cafe’s tables or taking your churros to go, you’ll appreciate the cafe’s chic atmosphere.
View this post on Instagram
Milk Beach
If you’re looking for a breathtaking spot to appreciate a cup of coffee or tea in London, look no further than Milk Beach. With stunning views of the cityscape and a relaxed vibe, Milk Beach is the ideal place to unwind and take in the beauty of London.
Milk Beach is located in Queens Park and Soho, two of the most popular neighbourhoods in London. Queens Park is known for its lively atmosphere and abundance of shops and restaurants, while Soho is a bit more laid-back with its art galleries and cafes. Regardless of which location you choose, you’ll be treated to stunning views of the city.
The best way to get to Milk Beach is by public transportation. If you’re coming to the Queens Park branch, take the tube to Oxford Circus station and walk west for about 10 minutes.
If you’re coming to the Soho branch, take the tube to Piccadilly Circus station and walk south for about 5 minutes. You can also take a bus to either Queens Park or Soho, but keep in mind that traffic can be heavy during peak hours.
In addition to its stunning views, Milk Beach is also known for its relaxed atmosphere. Whether you’re looking to people-watch or simply enjoy some rest, peace and quiet, this is the place to do it. There’s also an abundance of food and drink options, so you can stay fueled up as you enjoy your day at the beach.
View this post on Instagram
L’ETO London
L’ETO London is a chain of cafes that can be found in five different locations throughout the city. The cafes are located in Soho, Brompton Road, King’s Road, Mayfair, and Belgravia. Each location is unique and offers its own special atmosphere.
L’ETO Soho Location
The Soho location is located right in the heart of London city and is perfect for people-watching. The cafe has large windows that let natural light flood in, making it a bright and airy space. The menu features classic British dishes with a modern twist.
View this post on Instagram
L’ETO Brompton Road Location
The Brompton Road location is slightly more formal than the other cafes, making it ideal for business meetings or a leisurely lunch. The decor is chic and understated, with dark wood furnishings and white walls. The menu features a selection of seasonal salads, sandwiches, and main dishes.
L’ETO King’s Road Location
The King’s Road location is perfect for a quick bite or a leisurely meal. The cafe has an outdoor seating area that is ideal for people-watching on a warm day. The menu features a selection of light snacks and main dishes.

L’ETO Mayfair Location
The Mayfair location is the most formal of all the cafes. The decor is elegant and luxurious, with chandeliers and plush furnishings. The menu features classic British dishes with a gourmet twist.

L’ETO Belgravia Location
The Belgravia location is perfect for afternoon tea or a light lunch. The cafe has an outdoor seating area that overlooks a beautiful garden. The menu features a selection of sandwiches, pastries, and cakes.
No matter what you’re searching for, you’re sure to find it at L’ETO London. With five locations throughout the city, there’s sure to be a cafe that’s just right for you. Whether you’re looking for somewhere to enjoy afternoon tea or somewhere to get a quick bite to eat, L’ETO London has got you covered.

Fait Maison
Fait Maison is a cafe located in London that is known for its stunning design and delicious food. The cafe has two locations on Gloucester Road and one in Kensington. If you’re on the lookout for a place to enjoy a good meal and relax, Fait Maison is definitely worth the trip.
The Gloucester Road locations are near Hyde Park, and the Kensington location is near Kensington Palace. The simplest way to get to Fait Maison is by public transportation. The closest tube station to the Gloucester Road location is Marble Arch, and the closest station to the Kensington location is Queensway.

Fait Maison is known for its stunning design. The interior of the cafe features an abundance of natural light, marble floors, and brass fixtures. The menu at Fait Maison features classic French dishes with a modern twist.
View this post on Instagram

Tiffany Blue Box Cafe at Harrods
The Tiffany Blue Box Café at Harrods in London is a beautiful break from a bustling city. The pastel blue walls and plush seating make it feel like you’ve been transported to another world, and the food is absolutely divine.
If you’re not familiar with Harrods, it’s one of the most prominent department stores in the world, and it’s located in the posh Knightsbridge neighbourhood. While getting to Harrods may require a bit of effort, it’s definitely worth it once you see the Tiffany Blue Box Café in all its glory.

The best way to get to Harrods is by public transportation. If you’re coming from central London, take the Piccadilly line on the Underground (London’s subway system) to Knightsbridge station. From there, it’s just a short walk to Harrods.
Aside from its namesake colour, the Tiffany Blue Box Café is filled with beautiful antiques and art pieces. The café itself is quite small, but it feels cosy and inviting thanks to its intimate setting.
The menu features classic British dishes with a modern twist, and there’s even a section devoted entirely to sweets—perfect for those with a sweet tooth. Whether you want a quick, simple bite or a leisurely meal, the Tiffany Blue Box Café is sure to please.
View this post on Instagram
Saint Aymes
Have you ever wanted to visit the prettiest café in London? Well, now you can! Saint Aymes is a beautiful pastel and floral-themed café located on Connaught Street. The café offers a variety of 24-carat gold-smothered goodies, from hot chocolate to cakes. If it’s luxury that you’re looking for, then you will be in the right place.

The most suitable way to get there is by taking the Tube to Marble Arch Station. From there, it is only a 5-minute walk to the café. The décor of Saint Aymes is what makes it so beautiful.

The pastel colours and floral theme give the café a delicate and ethereal feeling. The 24-carat gold-smothered goodies are also a sight to behold! The Café’s delicate décor and luxurious offerings are sure to please. So, next time you’re in London, be sure to pay a visit to this magical place.
View this post on Instagram
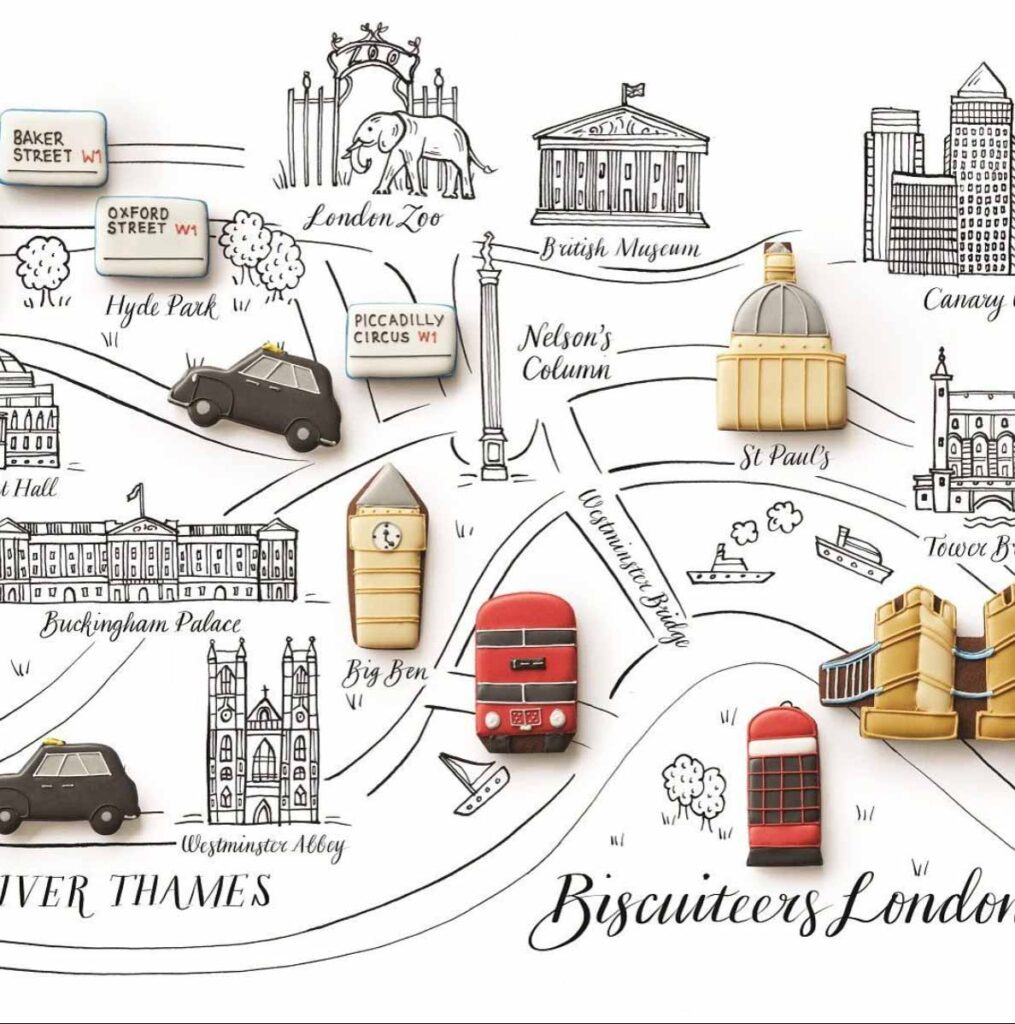
Biscuiteers
Biscuiteers, a cafe specialising in beautifully iced biscuits, have a branch located at Belgravia and Notting Hill in London. This cafe is the perfect place to enjoy a delicious treat or pick up a uniquely decorated gift.
The first thing you’ll notice when you walk into the Biscuiteers Boutique Icing Cafe is the eye-catching decor. The walls are covered in murals of pretty flowers and birds, and the shelves are lined with jars of colourful icing and boxes of biscuits. The overall effect is charming and inviting.
View this post on Instagram

Palm Vaults
Palm Vaults is a stunning cafe located in the heart of London. This hidden gem is known for its beautiful interiors and delicious food.
Palm Vaults is located in Shoreditch, which is in the East End of London. If you’re familiar with the city, it’s near Old Street station. If you’re not familiar with London, don’t worry – it’s easy to get to! Shoreditch is a vibrant and trendy area, so there are plenty of activities to do before or after you make your visit to Palm Vaults.
The best way to get to Palm Vaults is by public transport. Old Street station is served by both the Northern and Victoria lines, so it’s easy to reach from anywhere in the city. Once you exit the station, simply walk towards Great Eastern Street, and you’ll see Palm Vaults on your left-hand side.
PalmVaults has an Instagrammable interior with beautiful palm leaf wallpaper, hanging plants, and vintage furniture. The cafe also has an outdoor seating area which is perfect for people-watching on a sunny day. Not to mention, the food is absolutely delicious! They have a range of breakfast options as well as sandwiches, salads, and cakes.
View this post on Instagram
Daisy Green Collection
If you’re on the lookout for a little slice of Australia in the heart of London, look no further than Daisy Green Collection. This chain of cafés and restaurants serves up great coffee, amazing all-day brunch, and fab cocktails, all with an Aussie twist.
And with branches in locations like Bishopsgate, St. Johns Wood, Richmond, Paddington, Marylebone, Soho, Regent Street, Victoria, Barbican, Broadgate Circle, and Southbank, there’s sure to be a Daisy Green Collection café near you.
The first thing you’ll notice when you walk into a Daisy Green Collection café is the bright and airy atmosphere. The décor is inspired by Australian beach houses, with whitewashed walls and natural materials like wood and rattan. And, of course, there’s plenty of greenery everywhere you look.
But it’s not just the décor that makes Daisy Green Collection so beautiful – it’s also the food. The menu features all your Aussie favourites, like avocado toast and smashed peas on sourdough bread, as well as heartier options, like slow-cooked lamb shoulder with rosemary potatoes. And, of course, there are plenty of sweet treats on offer, too – we recommend the chocolate brownie!
View this post on Instagram
Finally, no visit to Daisy Green Collection would be done without trying one of their famous cocktails. The cocktail menu changes seasonally, but you can always expect refreshing drinks made with fresh ingredients. Our personal favourite is the Watermelon Martini – it’s the perfect summertime treat!
Getting to Daisy Green Collection is easy – just hop on the tube or take a bus to one of the many central London locations. Trust us, it’s worth the trip.